The Coronavirus disease 2019 (COVID-19) pandemic began at the end of 2019 in China and has quickly spread globally. Millions of people around the world are infected and hundreds of thousands have died.1 The clinical manifestations of COVID-19 vary from asymptomatic forms to severe clinical conditions characterized by respiratory failure, sepsis, septic shock and multiple organ dysfunction syndromes. Understandably, medical professionals and public health specialists are focused on taking care of individuals who are very sick, while containing the coronavirus’s spread in the general population. Less attention is given to the psychiatric consequences of the COVID-19 crisis.
Across the country, mental health experts were having to deal with an increasing number of people, particularly the youth ..It found that JOB LOSS or fear of it, STRESS, ISOLATION, LONELINESS, GRIEF at the loss of loved ones and FINANCIAL INSECURITY were factors leading to SUICIDES
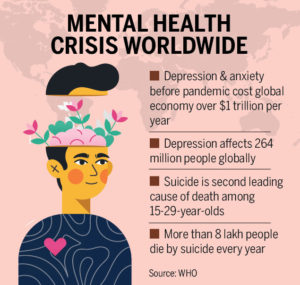
Multiple lines of evidence indicate that the COVID-19 pandemic has profound psychological and social effects. There is a pervasive awareness of uncertainty over the future and an understanding that the pandemic is far from over. It is possible that there will be economic privation and political upheaval. The psychological sequel of the pandemic will probably persist for months and years to come.
COVID-19 pandemic may increase the prevalence of psychiatric disorders and suicide rates during and after the pandemic.
Nothing in our lifetimes can be compared with the magnitude of the COVID-19 disaster. The last comparable crisis was the pandemic of Spanish Flu in 1918–19 caused by H1N1 viruses with genes of avian origin. About 500 million people or one-third of the world’s population were infected with the Spanish Flu viruses and at least 50 million people perished around the world including about 675 000 in the USA. The Spanish Flu epidemic was associated with an increase in death by suicide. It has been proposed that a decrease in social integration and interaction during the epidemic and the fears caused by the epidemic likely increased suicide. It is important to note that social isolation and fears are common during the current epidemic.
Studies indicate that the COVID-19 pandemic is associated with distress, anxiety, fear of contagion, depression and insomnia in the general population. Health care professionals are especially distressed.
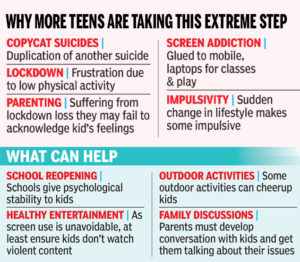
Social isolation, anxiety, fear of contagion, uncertainty, chronic stress and economic difficulties may lead to the development or exacerbation of stress-related disorders and suicidal, in vulnerable populations including individuals with pre-existing psychiatric disorders, low-resilient persons, individuals who reside in high COVID-19 prevalence areas and people who have a family member or a friend who has died of COVID-19. Individuals with pre-existing psychiatric disorders include not only patients who are treated by mental health professionals but also a very large number of people with psychiatric conditions who do not receive psychiatric treatment. Community epidemiological research in the USA shows that a majority of individuals with mood disorders are either untreated or undertreated.
Cases have surged, lockdowns have been imposed all over again. The measures, economists say, are forcing millions of households into poverty and contributing to a long-running tragedy: farmer suicides. Farm bankruptcies and debts have been the source of misery in the country for decades, but experts say the suffering has reached new levels in the pandemic.
The number of suicides might rise. The impact of the Covid-19 crisis on the agriculture sector will continue for at least the next couple of years and farmers will be pushed into more distress.
There is no market for the produce. Not even 10 per cent of farmers’ produce has been sold during the lockdown and farmers have no money for sowing and to look after their families.
Individuals in suicidal crises need special attention. Some suicidal persons, might not seek help because of fear that attending face-to-face appointments with a health care professional might put them at risk of contracting COVID-19 or because of other reasons. Therefore, individuals with a recent suicide attempt history need a follow-up. Clinicians should have well-defined guidelines on how to deal with suicidal individuals.
Suicide prevention in the COVID-19 era is an important and difficult issue. Research studies are needed of how mental health consequences can be mitigated during and after the COVID-19 pandemic. It is to be hoped that the efforts of clinicians, researchers and policy makers will reduce COVID-19 related suicides.